Can progesterone help with Conception and Pregnancy problems?
I have so many women writing about just these problems. As it's something dear to my heart (I had five miscarriages before having my daughter) I have put together information on progesterone and conception and how to use it during pregnancy. You'll find this below together with a chapter from one of Dr Dalton's books on the role progesterone plays during pregnancy.
Progesterone is vital to pregnancy. In fact it's name means pro-gestation, an unfortunate name as it's other roles in the body tend to be forgotten. It was first extracted from the corpus luteum, so came be be regarded as a female hormone involved solely in reproduction.
Progesterone is not a sex hormone, it plays no part in the secondary sexual characteristics which develop at puberty. It is secreted primarily by the ovaries in females and the testes in men. Smaller amounts are produced by the adrenal glands, the brain and glial cells. There are no great quantitative differences between men and women (at least outside the luteal phase). It is the precursor to the sex hormones oestrogen and testosterone, and to cortisol and aldosterone.
Progesterone regulates gene expression, has a positive fundamental effect on cell differentiation and growth, with anti-oxidative and autoimmune anti-inflammatory mechanisms. It positively effects the nervous system by stimulating neurotrophic factors, quenching oxidative hyperactivity and regulating autoimmune responses.
Menstrual cycle
Normal monthly cycles can vary from as little as twenty one days to as long as thirty five, the average being twenty eight. Cycles outside this range are generally regarded as abnormal. For more information on this see the pages on Menstruation and PCOS.
The first half of the monthly cycle is known as the follicular or proliferative phase, and can last from 7 to 59 days, although the norm is 12-21 days. A long follicular phase is defined as lasting 24 days or longer. Oestrogen is the dominant hormone.
The second half of the menstrual cycle is called the luteal or secretory phase. All women, irrespective of the length of their cycle, should start ovulating 12 to 14 fourteen days before the next menstruation. Progesterone is the dominant hormone.
Oestrogen is a mitogen, it stimulates cells to proliferate i.e. to divide and multiply. Progesterone stops mitosis and causes differentiation.
At the beginning of the follicular phase, in response to FSH made by the pituitary gland, a few to several hundred eggs start developing. Each egg is contained in a cyst called a Graafian follicle, which starts making oestrogen, this in turn causes the egg to grow and mature. Oestrogen also stimulates the endometrium (lining of the uterus) to grow and thicken. When one or possibly two eggs are fully developed they rise to the surface of the ovary and appear as small 'blisters'.
At the beginning of the cycle, ie day 1 of bleeding, oestradiol production either drops slightly or is flat for the first 2-4 days. It then rises slowly for the next 6-10 days, and then sharply for 2-5 days. This is the preovulatory peak, after which it drops.
During the fifty hours prior to the mid-cycle surge, oestradiol, progesterone and another pituitary hormone secreted by the anterior pituitary gland called LH (luteinising hormone) begin rising, while FSH declines.
The cells forming the outer layer of the Graafian follicle are called thecal cells. LH is required for both the growth of preovulatory follicles and ovulation of the dominant follicle. Under the influence of LH they secrete testosterone. LH causes proliferation, differentiation, and secretion of androgens by the theca cells which surround the ovum, giving rise to androgen levels.
The androgens, notably androstendione, migrate from the theca cells to the granulosa cells where they are converted by the enzyme aromatase into oestrogen, particularly oestradiol. The theca cells also produce oestradiol without the need for conversion.
This rise in the androgens is responsible for the acne, oily skin, facial hair, loss of scalp hair etc., that some women experience.
12 hours prior to the mid-cycle surge, progesterone rises exponentially. This surge is produced by brain cells, and has nothing to do with the surge that occurs after ovulation. It's thought to initiate the LH surge which begins 12 hours after the progesterone surge. FSH rises again at the same time as LH.
This preovulatory surge in progesterone is now known to be essential for the facilitation of feminine sexual behaviour too.
The surge of the gonadotrophins causes oestradiol levels to rapidly fall, while progesterone continues to rise. The gonadotrophins plateau for about 14 hours after which they drop sharply.
Androstenedione (A) and testosterone (T) increase at a slow rate before the surge, rising faster when the mid-cycle surge begins. Then about fourteen hours after initiation of the surge, they decline, but at a slower rate than oestradiol. In spite of the significant increase in A and T, oestradiol still plummets. It's thought that the rapid rise in progesterone may inhibit aromatase activity.
Ovulation
Ovulation occurs approximately 10-12 hours after the LH peak and 24-36 hours after the oestrogen peak. The Graafian follicle ruptures, releasing the egg. The follicle is now called the corpus luteum due to its yellow colour.
For the next twelve to fourteen days the corpus luteum secretes progesterone, which rises steeply until 6-7 days after ovulation when it peaks. The peak lasts for about 3-4 days, when progesterone declines sharply, after which menstruation occurs. The corpus luteum is able to synthesise upwards of 40 mg of progesterone on a daily basis. Although the range is normally 5-20mg per day.
It's been found that progesterone is capable of stimulating it's own synthesis. The typical negative feedback system seen in other endocrine tissues does not operate in the corpus luteum, and at the end of the luteal phase, in spite of LH secretion, the corpus luteum regresses and progesterone secretion declines.
Therefore using progesterone at ovulation will enhance the early rise in progesterone so vital for successful implantation. In fact using it within the 12 hours of the pre-ovulatory surge will enhance ovulation, and ensure there's an early rise.
If fertilisation has occurred, progesterone will continue rising. In order to do so, the corpus luteum needs stimulus from a fertilised egg, under the influence of hCG (human chorionic gonadotrophin).
The corpus luteum also produces androgens, oestrogens, 20alpha-hydroxyprogesterone, and 5alpha-reduced progesterones.
Although the corpus luteum is influenced by LH, insulin is also required. It regulates luteal cell function and causes an increase in progesterone secretion. Insulin also stimulates a substantial increase in oestradiol in the presence of androstenedione. LDL cholesterol is known to be critical for progesterone production, whereas HDL is ineffective.
Under the influence of progesterone the lining of the uterus has stopped proliferating, instead becoming a spongy layer ready for the egg to embed itself.
After intercourse, when millions of sperm enter the vagina, and make their way through the cervix, through the uterus and into the Fallopian tubes, fertilisation takes place when a sperm embeds itself into an egg.
Low progesterone levels in the very early days of the luteal phase makes fertilisation less certain.
Progesterone is essential for sperm capacitation and the acrosome reaction.
The now fertilised egg continues on it's journey up the Fallopian tube until it reaches the uterus, where it becomes embedded in the endometrium (lining of the uterus). If fertilisation has taken place, the corpus luteum continues to make progesterone for about three months. This is dependant on stimulation by hCG, which is produced by the developing embryo, and later by the placenta.
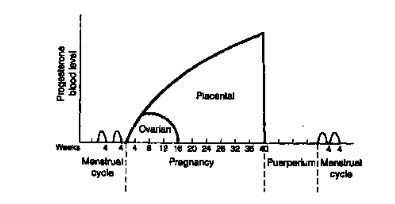
During this time the placenta is developing and at about two months starts secreting progesterone, and continues to do so until birth.
Vitamin D is also vital for ovulation, a lack causing anovulatory cycles. Other nutrients vital for ovulation are N-acetylcysteine, arginine and inositol. If insufficient levels of these are present, anovulatory cycles can also occur.
A defective luteal phase
All women, irrespective of the length of their cycle, should start ovulating twelve to fourteen days before the next menstruation. If shorter, there is insufficient time for the endometrium to be readied for the embryo to implant, this is known as a defective luteal phase.
If the corpus luteum does not make sufficient progesterone during these twelve to fourteen days, it will also result in a defective luteal phase. Symptoms are spotting during the entire luteal phase, or for a few days before full bleeding occurs. It appears to be a problem found in many women now and could well be due to the Endocrine Disruptors in the environment. Other factors are discussed on the Infertility page.
Research has found that a steeper early luteal rise in progesterone and higher mid-luteal progesterone and oestrogen concentrations make for successful implantation.
Many so called 'infertile' women are not. Conception could be taking place each month, but unless there's a steep early luteal phase rise in progesterone, implantation will be unlikely.
Contraceptives can cause a severe disruption in the cycle after discontinuing them. It's essential to give enough time for the synthetic oestrogens and progestins to diminish, before attempting conception.
How to use progesterone to extend the luteal phase
A low dose of progesterone will not help. 100-200mg/day or more progesterone should be used, depending on symptoms. In some cases up to 400mg/day will be needed. It should be used from ovulation, or during the 50 hour pre-ovulatory surge.
If used too early i.e. 7 to 8 days before ovulation, which is when many women are told to start it, progesterone can act as a contraceptive, but usually 200mg/day or more are needed. So starting too early can prevent the chance of falling pregnant.
When to start using progesterone
It is advisable to start the progesterone well before pregnancy to allow the body to adjust. Many women are started on progesterone many days, often weeks after they fall pregnant and suffer oestrogen dominance symptoms. It's bad enough suffering from these when first pregnant, but twice?! For more info please see the page on Oestrogen Dominance.
How to check when ovulation has occurred
Taking temperature readings or using a mini microscope will help to check for ovulation, the mini microscope is more reliable, as temperature can vary from as little as 0.5 degrees to 5 degrees.
Saliva or vaginal mucus is used for the test, by dabbing a small amount on the end of the microscope. During the follicular phase, the pattern formed by the saliva/mucus is spotty, as ovulation draws near a fern like pattern starts emerging, becoming completely fern like when ovulation has occurred, returning to the spotty pattern almost immediately. For more information see Ovulation Microscope.
Normal oral body temperature in adult men and women ranges between 33.2-38.2°C (92-101°F). Typical average temperatures are 37.0°C (98.6°F).
In women it varies between the follicular and the luteal phase. During the follicular phase, i.e. from the first day of menstruation to ovulation, it ranges from 36.45 to 36.7°C (97.6 to 98.1°F).
During the 12-14 day luteal phase, i.e. after ovulation to menstruation, temperature increases by 0.15 - 0.45°C (0.2 - 0.9°F) due to the increased metabolic rate caused by rapidly rising levels of progesterone. Temperature ranges between 36.7 - 37.3°C (98.1 - 99.2°F) during the luteal phase, but drops down to follicular levels within a few days of bleeding.
Fertilisation
One of the most important things to remember about conception is the life span of the sperm and ovum. The average life of the sperm appears to be two to three days, sometimes longer, but the ovum only lives twelve hours and in rare cases twenty four hours.
All research points to a greater success in conception if intercourse takes place in the one to two days prior to ovulation, when the fern like pattern is almost complete. This is during the preovulatory progesterone surge.
This allows time for the sperm to travel through the uterus and up the Fallopian tubes to meet the egg before it becomes over mature or it dies. One of the problems with an over mature egg is it diminishes the chances of fertilisation, can result in a miscarriage or result in foetal abnormalities. The health of the future child is dependant on these factors.
The nearer intercourse takes place to ovulation, the greater the chances of conception.
Pregnancy
It must be remembered that twelve to fourteen days is necessary for the lining to mature enough to receive a fertilised egg. If bleeding does occur, it means the egg has not been fertilised or implantation has not taken place. The progesterone should then be stopped and only started again at the next ovulation. If bleeding does not start fourteen days later, it is possible that fertilisation and implantation have occurred.
On no account must the progesterone be stopped at this stage, otherwise it could cause a miscarriage.
If there is no menstruation and pregnancy is confirmed, the progesterone should be continued, using between 100-200mg/day or more until the fourth month. After the critical stage has passed the progesterone it can be tapered off slowly, or can be continued until birth.
The majority of women are advised to stop cold turkey, this is not advisable. Progesterone withdrawal can not only cause a miscarriage if the placenta is making insufficient at this point. But other adverse symptoms can occur. These are the same as those experienced due to progesterone withdrawal the few days prior to bleeding during the monthly cycle.
If tapering off, the amount should be reduced very slowly, taking about a month to do so. This is easy to do if using a progesterone cream, difficult if using injections or suppositories. Either switch to a cream, or in the case of injections withdraw slightly less progesterone from the vial for each reduction. In the case of suppositories, divide them into 25mg pieces, adjusting the tapering by using as many pieces as required.
It's advisable to continue using progesterone until birth if there's a likelihood of a pre-term birth or pre-eclampsia.
Please monitor symptoms, and if spotting, headaches, water retention or nausea should occur increase the amount and continue using it till birth. In some women water retention and a rise in blood pressure sometimes occurs in the last one to two months, please increase the amount if this should happen.
If nausea occurs 400-800mg/day is needed to stop it.
It is the first three, possibly four months that are critical. 25% of miscarriages occur during the first six weeks when the child is still in the embryo stage. The risk drops to 8% after eight weeks, when the child is now termed a foetus.
During this time the placenta is developing and after about two months starts secreting progesterone, while ovarian production starts declining. If at this point placental production is insufficient to meet the demands of the growing foetus a miscarriage can occur. It is therefore advisable to continue with the supplemental progesterone until at least the third month. All being well the placenta continues to make progesterone in increasing amounts until birth, when levels drop abruptly with the expulsion of the placenta, or afterbirth as it's now generally termed.
Miscarriages and Pre-term births
Many factors cause miscarriages, far too many for here. But a few are chromosomal alterations, uterine anomalies, antiphospholipid antibodies, exposure to bisphenol A an endocrine disruptor, high alcohol intake, high levels of the inflammatory cytokines TNFa and IL-6, and natural killer cells, if activated by TNFa, may cause the death of the embryo. Progesterone suppresses TNFa and IL-6 activity, and excessive NK cell activity.
Of significance for this page are low levels of progesterone and Vitamin D, and high levels of oestrogen and free testosterone, often overlooked. A level of progesterone over 12.3 ng/ml in early pregnancy indicates a normal pregnancy.
A ratio of 1.05 or higher for free testosterone to total testosterone indicates a miscarriage is likely. But if the free testosterone ratio is lower than 0.84 a normal pregnancy occurs. The reasoning behind this is excess oestrogen causes foetal death. The enzyme 5-alpha reductase Type 1 mRNA is induced in the pregnant brain, this inactivates testosterone, which reduces the available substrate for oestrogen synthesis.
Progesterone also inhibits the enzyme aromatase, which effects the conversion of testosterone to oestrogen.
A short cervix increases the risk of pre-term births, progesterone reduces the risk.
It is also essential to bear in mind that stress can cause a miscarriage. The rise in cortisol in response to the stress, results in a drop in the progesterone level, this in turn can lead to spotting or a miscarriage. To prevent this, as soon as any stress is felt, increase the amount of progesterone till it has passed. If any anxiety is felt please look through this page.
Many women are devastated by a miscarriage, understandably, but none are warned that as many as 20% of all pregnancies end in a miscarriage within two weeks of fertilisation. Another 15% occur within the first fourteen weeks (three and half months).
A short cervix increases the risk of pre-term births, progesterone reduces the risk.
Preeclampsia
Studies have shown that low progesterone and vitamin D levels are found in preeclampsia. One study finding progesterone was 'pathologically and statistically' lower. Serum allopregnanolone (a potent metabolite of progesterone) was found to be significantly lower too. The Th1 (inflammatory cytokines) and Th2 (anti-inflammatory cytokines) play a role. The number of Th1 cells and the ratio of Th1:Th2 in preeclampsia is significantly higher than in a normal pregnancy. Progesterone and vitamin D both increase levels of Th2.
But a number of other factors have been found to play a role. Women with insulin resistance, high levels of malondialdehyde and homocysteine are at greater risk of developing preeclampsia. A lack of selenium and low levels of glutathione and other antioxidants increase the risk too.
If recurrent miscarriages, pre-term births or preeclampsia have occurred consider using 200-600mg/day progesterone. Many believe progesterone is not effective at preventing these, but the evidence points to far too little progesterone being used in the unsuccessful studies.
Depression
25% of women suffer some form of depression after child birth. From the 'baby blues', to post natal depression (PND), to post natal psychosis (PNP), which can result in infanticide and suicide. Luckily PNP only occurs in 0.05% of women. The depression is caused by the rapid drop in progesterone levels after the expulsion of the placenta. Serotonin levels drop too. Anti-depressants are not required, what is are large amounts of progesterone. From 800mg/day for PND up to 2400mg/day for post natal psychosis, the amounts Dr Dalton found effective.
To recap...
- Progesterone must only be used at ovulation, or during the 50 hour preovulatory surge if pregnancy is the aim
- Take temperature readings or use a mini microscope to help check for ovulation
- On no account must the progesterone be stopped if conception is suspected, otherwise it could cause a miscarriage
- It is essential to continue the progesterone over the first 2-3 month critical phase, particularly the first 2 months
- It is also essential to bear in mind that stress can cause a miscarriage
- The nearer intercourse takes place to ovulation, the greater the chances of conception
- Use at least 100-200mg/day progesterone, possibly more
- It should always be used a minimum of twice a day by dividing the amount
- Make sure sufficient nutrients are taken to support the pregnancy, particularly vitamin D and taurine
- Avoid all skin care, foods and drinks which contain endocrine disruptors and other toxins, these can cause epigenetic changes in the foetus
Drugs
Mention should be made of the drugs which are often given in place of progesterone to prevent miscarriages and pre-term births, in the mistaken belief they are one and the same. One is a synthetic progesterone called Duphaston which contains dydrogesterone. Another is 17-hydroxyprogesterone caproate (17-OHP-C), also a synthetic hormone.
But because they're progestins, they are not broken down into the normal progesterone metabolites, such as the all important allopregnanolone. These are as essential as progesterone itself, especially in pregnancy, when the foetus is particularly susceptible to toxins or a lack of necessary nutrients.
A metabolite of progesterone is sometimes used too, 17-Hydroxyprogesterone, this is natural, and increases during the third trimester. It's often called 17-OHP, or 17-OH, or 17-P.
No adverse side affects have been reported with the use of 17-OHP, which is produced primarily by the adrenal glands. But there are safety concerns about 17-OHP-C use. Progesterone is also more potent that 17-OHP-C.
OTC drugs
Many women take over-the-counter mild analgesics during pregnancy. Drugs such as acetaminophen (paracetamol), and non-steroidal anti-inflammatory drugs (NSAIDS) like ibuprofen and acetylsalicyclic acid (aspirin). These have been shown to increase the risk of congenital malformations, including cryptorchidism and hypospadia. Paracetamol in particular increased the risk of cryptorchidism as it's a potent inhibitor of androgen production.
hCG
hCG or human chorionic gonadotrophin is a hormone produced by the developing embryo after conception. Once the embryo has implanted a specialised part of the placenta takes over production. The role of hCG is to prevent the corpus luteum from disintegration. The corpus luteum is critical for the production of progesterone for the first 8 weeks, until the placenta begins to take over production. Please note that hCG starts dropping after 13 to 16 weeks GA as the corpus luteum is no longer needed.
GA: Gestational Age or LMP: Last Menstrual Period
It is standard practice to take the last menstrual period as the 'age' of the foetus. This is always regarded as occurring 14 days prior to ovulation. But foetal age can of course vary, as the menstrual cycle varies between 21 to 35 days. Ovulation occurring between days 7 to 21, and therefore conception occurring on or just after. If a woman has a longer or shorter cycle than 28 days, this should be taken into account.
Chart taken from Dr Dalton's book "Once a Month"...
Here's the link to the chapter from Dr Dalton's book 'PMS The Essential Guide to Treatment Options' on the role progesterone plays during pregnancy.
In memory of Dr Katherina (Kittie) Dalton.
To understand the hormonal changes in pregnancy please see the page on Hormone Testing.
Additional information
The growing foetus is an extra burden on the mother, so it is essential to make sure all nutrients the foetus needs are available.
Please consider taking the following each day...
- 5 000iu's/day vitamin D3 (cholecalciferol) vital for a developing foetus, to prevent miscarriages, epigenetic changes, rickets, heart failure, epilepsy, Type 1 diabetes, and upper respiratory track infections in the newborn, to reduce the risk of preeclampsia in the mother
- 1000-2000mg/day taurine to prevent epilepsy, insulin resistance, impaired glucose tolerance, diabetes, impaired neurological function, vascular dysfunction and growth retardation in the developing foetus and newborn. Taurine is not found in grains, legumes, vegetables, nuts, seeds or fruit, only animal protein.
- 5ml Omega 3 fish oil, particularly DHA, needed by the developing brain
- Vitamin B complex with extra folic acid bringing this up to 800mcg/day to prevent neural tube defects. If a vegetarian, please be cautious, as excess folic acid masks a B12 deficiency. A lack of B12 in utero increases the risk of insulin resistance in the child.
Do not take cod liver oil, or any fish liver oil. The excessive vitamin A it contains prevents vitamin D from being absorbed. Take beta-carotene if short of vitamin A.
To clear any confusion, 'fish oil' comes from the muscle of the fish and contains Omega 3. Fish 'liver' oil obviously comes from the liver, it contains large amounts of vitamin A and very small amounts of vitamin D. There is a world of difference between the two.
For more info on vitamin D levels, test kits etc see...
Blood levels should be 70-100ng/ml (175-250nmol/L) and not the 30ng/ml (75nmol/L) most labs and doctors regard as adequate. The minimum daily dose should be 5000iu's per day, although recent research indicates it should be 10,000iu's per day, see here.
Read all labels on containers, especially those for food and cosmetics. Look for natural alternatives to body care products, many contain high levels of endocrine disruptors and carcinogens, particularly the sunscreens.
Please see Our Stolen Future for more information on endocrine disruptors.
Please see the page on Nutrition for more information about food.
For more information on pregnancy see..
Please see these excellent videos on pregnancy and vitamin D...
Carol. L Wagner, M.D., Ph.D. - Pregnancy and Lactation
Vitamin D supplementation in pregnancy & breastfeeding - effectiveness and safety. Dr Bruce Hollis
Reference papers
Townsend Letter April 2013
Integrative Approaches to Infertility for Women
American Congress of Obstetricians and Gynecologists (ACOG) 61st Annual Clinical Meeting May 08, 2013
Low-Carb Diet Improves In Vitro Fertilization
The Journal of Clinical Endocrinology & Metabolism November 16, 2012 jc.2012-3275
Maternal Serum 25-Hydroxyvitamin D and Measures of Newborn and Placental Weight in a U.S. Multicenter Cohort Study
Hum. Reprod. (2013) 28 (1): 77-86
Sex-specific effect of first-trimester maternal progesterone on birthweight
Am J Obstet Gynecol 2012
Both Vaginal Progesterone and Cerclage Curb Preterm Birth
Hum Reprod. 2012;27(11):3321-3327
Characterizing the Influence of Vitamin D Levels on IVF Outcomes
Eur J Endocrinol. 2012 May;166(5):765-78
Vitamin D and fertility: a systematic review
European Association for the Study of Diabetes October 3, 2012
Low First-Trimester Vitamin D Predicts Gestational Diabetes
BMJ 2012; 345 Published 27 September 2012
Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies
Pediatrics 2012;129:e1552-e1561
Increased Cardiovascular Risk Factors in Offspring of Preeclamptic Mothers
Stroke. 2011; 42: 2564-2570
Trends in Pregnancy Hospitalizations That Included a Stroke in the United States From 1994 to 2007
ScienceDaily (July 28, 2011)
Rate of Stroke Increasing Among Women During, Soon After Pregnancy
ScienceDaily (Mar. 10, 2009)
Migraines Increase Stroke Risk During Pregnancy
Arch Dis Child. May 23, 2012
Caesarean Delivery May Predispose Children to Obesity
ScienceDaily (Dec. 1, 2010)
Recurrent Miscarriage Raises Heart Attack Risk Fivefold in Later Life, Study Finds
Heart 2011;97:49-54
Pregnancy loss and risk of cardiovascular disease: a prospective population-based cohort study (EPIC-Heidelberg)
Human Reproduction. 2012;27(4):1191-1201
Intrauterine Exposure to Mild Analgesics During Pregnancy and the Occurrence of Cryptorchidism and Hypospadia in the Offspring
Women's Health Issues. 2012;22:e73-e81
Births Attended by Midwives Safe, Need Fewer Interventions
J Perinatol. 2011 Jan 20
Vitamin D supplementation during pregnancy: safety considerations in the design and interpretation of clinical trials
CMAJ. 2011 March 22; 183(5): 549555
Maternal selenium status during early gestation and risk for preterm birth
Am J Obstet Gynecol 2011
IM Progesterone Won't Delay Delivery After Arrest of Preterm Labor
Heart 2010;97:49-54
Pregnancy loss and risk of cardiovascular disease: a prospective population-based cohort study (EPIC-Heidelberg)
Science Daily Dec. 2, 2010
Recurrent Miscarriage Raises Heart Attack Risk Fivefold in Later Life, Study Finds
The Journal of Clinical Endocrinology & Metabolism November 1, 2010 vol. 95 no. 11 5105-5109
A Nested Case-Control Study of Midgestation Vitamin D Deficiency and Risk of Severe Preeclampsia
Journal of Bone and Mineral Research, 2010, Volume 25, Issue 1 (p 14-19)
Low Maternal Vitamin D Status and Fetal Bone Development: Cohort Study
Journal of Bone and Mineral Research, 2010, Volume 25, Issue 1 (p 11-13)
Vitamin D Insufficiency and Skeletal Development In Utero
Ann Rheum Dis doi:10.1136/ard.2010.134817
Vitamin D: an instrumental factor in the anti-phospholipid syndrome by inhibition of tissue factor expression
GrassrootsHealth April 30, 2010
Researchers Recommend Pregnant Women Take 4,000 IU Vitamin D a Day
The British Journal of Dermatology. 2010;163(3):616-623
Probiotics in Pregnant Women to Prevent Allergic Disease: A Randomized, Double-blind Trial
Ann Rheum Dis doi:10.1136/ard.2010.134817
Vitamin D: an instrumental factor in the anti-phospholipid syndrome by inhibition of tissue factor expression
Arch Gen Psychiatry. 2010 Oct;67(10):1012-24
A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction
Medscape October 14, 2010
ACOG Guidelines for Treating Nausea and Vomiting in Pregnant Women Reviewed
Amer J Perinatol 2010; 27(2): 157-162
Uterine Activity in Women Receiving 17 -Hydroxyprogesterone Caproate for the Prevention of Preterm Birth: An Observational Study
BJOG. 2009 Oct;116(11):1515-9
Low saliva progesterone concentrations are associated with spontaneous early preterm labour (before 34 weeks of gestation) in women at increased risk of preterm delivery
J Perinat Med. 2009;37(4):338-42
Progesterone induced blocking factor (PIBF) and Th1/Th2 cytokine in women with threatened spontaneous abortion.
Brain Behav Immun. 2009 August; 23(6): 750754.
Depressive symptoms are associated with elevated serum proinflammatory cytokines among pregnant women
Clin Endocrinol (Oxf). 2009 Mar;70(3):372-7
Vitamin D, PTH and calcium levels in pregnant women and their neonates
J Reprod Immunol. 2009 Jul;81(1):17-24
Calcitriol inhibits TNF-alpha-induced inflammatory cytokines in human trophoblasts
Human Reproduction Update 2009 15(1):119-138
Non-genomic progesterone actions in female reproduction
Journal of Obstetrics & Gynaecology 2009, Vol. 29, No. 6, Pages 493-498
Intravaginal use of natural micronised progesterone to prevent pre-term birth: A randomised trial in India
Ther Clin Risk Manag. 2009; 5: 5564
Progesterone for the prevention of preterm birth: indications, when to initiate, efficacy and safety
Hypertension. 2009;53:805-811
Cardiovascular Effects of Physiological and Standard Sex Steroid Replacement Regimens in Premature Ovarian Failure
J Reprod Immunol. 2009 Jun;80(1-2):91-92009
Progesterone-induced blocking factor (PIBF) modulates cytokine production by lymphocytes from women with recurrent miscarriage or preterm delivery
Endocrine Abstracts (2009)
Prolonged treatment with N-acetylcysteine and L-arginine restores gonadal function in patients with PCO syndrome
International Journal of Fertility and Sterility Vol 3, No 2, Aug-Sep 2009, Pages: 66-73
N Acetyl Cysteine, A novel Remedy for Poly Cystic Ovarian Syndrome
Rev Med Liege. 2008 Feb;63(2):87-91
Vitamin D deficiency in recently pregnant women
Hum. Reprod. July 23, 2008
Soy food and isoflavone intake in relation to semen quality parameters among men from an infertility clinic
Frontiers in Bioscience 13, 985-994, January 1, 2008
Cytokine imbalance in pregnancy complications and its modulation
Advances in Experimental Medicine and Biology Volume 643, November 05, 2008
Taurine Supplementation and Pancreatic Remodeling
Hum. Reprod. Advance Access published online on December 3, 2008
Rates of preterm birth following antenatal maternal exposure to severe life events: a population-based cohort study
Diabetologia Volume 51, Number 1 / January, 2008
Vitamin B and folate concentrations during pregnancy and insulin resistance in the offspring: the Pune Maternal Nutrition Study
NEJM Volume 357:462-469 August 2, 2007 Number 5
Progesterone and the Risk of Preterm Birth among Women with a Short Cervix
Ultrasound Obstet Gynecol. 2007 Oct;30(5):697-705
Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo- controlled trial
Hum. Reprod. Advance Access published online on January 16, 2007
Effect of oral administration of dydrogestrone versus vaginal administration of natural micronized progesterone on the secretory transformation of endometrium and luteal endocrine profile in patients with premature ovarian failure: a proof of concept
J Matern Fetal Neonatal Med. 2007 Feb;20(2):89-112
Embryo-fetal toxicity signals for 17alpha-hydroxyprogesterone caproate in high-risk pregnancies: a review of the non-clinical literature for embryo-fetal toxicity with progestins
J Clin Invest. 2007 Jul;117(7):1824-34
FKBP52 deficiency-conferred uterine progesterone resistance is genetic background and pregnancy stage specific
The Journal of Clinical Endocrinology & Metabolism September 1, 2007 vol. 92 no. 9 3517-3522
Maternal Vitamin D Deficiency Increases the Risk of Preeclampsia
Eur J Clin Nutr. 2007 Sep;61(9):1136-9
Does vitamin D supplementation in infancy reduce the risk of pre-eclampsia?
Medscape November 6, 2007
New Studies Strengthen Preeclampsia/CVD
Rheumatology 2007 46(10):1517-1519
Recurrent spontaneous abortions in antiphospholipid: natural killer cells an additional mechanism in a multi factorial process
American Society for Nutrition J. Nutr. 137:1887-1894, August 2007
Enzymes of the Taurine Biosynthetic Pathway Are Expressed in Rat Mammary Gland
Hum. Reprod. (January 2006) 21 (1): 46-51
Progesterone enhances HLA-G gene expression in JEG-3 choriocarcinoma cells and human cytotrophoblasts in vitro
N Z Med J. 2006 Sep 8;119(1241):U2144
Vitamin D deficiency in pregnant New Zealand women
Australian and New Zealand Journal of Obstetrics and Gynaecology Volume 46, Issue 2, pages 7783, April 2006
Endogenous anti-oxidants in pregnancy and preeclampsia
J Clin Endocrinol Metab. 2005 Feb;90(2):944-52
Placental expression of IFN- and its receptor IFN- R2 fail to switch from early hypoxic to late normotensive development in pre-eclampsia
Immunology of Pregnancy, 2005, vol 89, pp 49-61
Immunology of Preeclampsia
IJMS Vol 30, No 4, December 2005
Evaluation of Androgen and Progesterone Levels in Women with Preeclampsia
Human Reproduction 2005 20(7):2035-2036
Recurrent miscarriage and embryonic loss
BJOG Volume 112, pages 5760, March 2005
The changing role of progesterone in preterm labour
Nutrition Reviews Volume 63, Issue 7, pages 225 232, July 2005
Vitamin D for the Prevention of Preeclampsia? A Hypothesis
Human Reproduction 2005 20(8):2325-2329; doi:10.1093/humrep/deh888
Exposure to bisphenol A is associated with recurrent miscarriage
Emory University Health Sciences Center 09 Feb 2005
Sex hormone metabolite reduces stress, anxiety in female rats
Brain Res (2005) 1043: 76-86
Progesterone regulation of catecholamine secretion from chromaffin cells
Akush Ginekol (Sofiia). 2004;43(5):22-4
Utrogestan and high risk pregnancy
Horm Behav (2004) 46: 467-73
Acute progesterone can recruit sex-specific neurochemical mechanisms mediating swim stress-induced and kappa-opioid analgesia in mice
Lupus. 2004;13(9):639-42
Progesterone supplement in pregnancy: an immunologic therapy?
Lupus September 2004 vol. 13 no. 9 630-634
Cytokines in recurrent miscarriage
Exclusive from New Scientist Print Edition 12 November 2004
Stress can make pregnant women miscarry
The American Journal of Cardiology Volume 93, Issue 6, 15 March 2004, Pages 805-808
Risk for subsequent coronary artery disease after preeclampsia
Lupus September 2004 vol. 13 no. 9 635-638
Sex hormones influence on the immune system: basic and clinical aspects in autoimmunity
Diabetologia Volume 47, Number 10 / October, 2004
Taurine supplement in early life altered islet morphology, decreased insulitis and delayed the onset of diabetes in non-obese diabetic mice
Occupational and Environmental Medicine 2004; 61 :1021-1026
Stress and dysmenorrhoea: a population based prospective study
American Journal of Obstetrics and Gynecology Volume 188, Issue 2 , February 2003, Pages 419-424
Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: A randomized placebo-controlled double-blind study
Journal of Reproductive Immunology Volume 59, Issue 2, August 2003, Pages 161-173
Th1/Th2 balance in preeclampsia
Human Reproduction, Vol. 17, No. 10, 2580-2584, October 2002
Depression as a potential causal factor in subsequent miscarriage in recurrent spontaneous aborters
Journal of Perinatal Medicine. 2002, Volume 30, Issue 4, Pages 281286
Taurine and taurine-deficiency in the perinatal period
American Journal of Reproductive Immunology, Volume 46, Number 2, August 2001, pp. 117-123(7)
Stress and Pregnancy Loss: Role of Immune Mediators, Hormones and Neurotransmitters
J Clin Endocrinol Metab. 2000 Jul;85(7):2429-33
Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients
Hum Reprod. 2000 Jun;15 Suppl 1:46-59
Progesterone inhibits in-vitro embryotoxic Th1 cytokine production to trophoblast in women with recurrent pregnancy loss
FrontiersinNeuroendocrinology 21,156(2000)
Neurosteroids: Biosynthesis and Function of These Novel Neuromodulators
Fertil Steril. 1999 Jan;71(1):40-9
Preimplantation urinary hormone profiles and the probability of conception in healthy women
Clin Exp Immunol. 1999 September; 117(3): 550555
Quantitative analysis of peripheral blood Th0, Th1, Th2 and the Th1:Th2 cell ratio during normal human pregnancy and preeclampsia
Psychiatric Clinics of North America Volume 21, Issue 2, 1 June 1998, Pages 309-323
PSYCHONEUROENDOCRINOLOGY OF DEPRESSION Hypothalamic-Pituitary-Gonadal Axis
BJOG: Volume 105 Issue 10 Page 1082 - October 1998
A double-blind randomised placebo controlled trial of postnatal norethisterone enanthate: the effect on postnatal depression and serum hormones
Hum Reprod. 1997 Dec;12(12):2607-13.
Preimplantation hormonal differences between the conception and non-conception menstrual cycles of 32 normal women
Eur J Obstet Gynecol Reprod Biol. 1996 Jul;67(1):5-8
The prognostic value of serum estradiol, progesterone, testosterone and free testosterone levels in detecting early abortions
Br J Obstet Gynaecol. 1995 May;102(5):364-9
The role of a single progesterone measurement in the diagnosis of early pregnancy failure and the prognosis of fetal viability
J Immunol. 1995 Jul 1;155(1):128-33
Progesterone favors the development of human T helper cells producing Th2-type cytokines and promotes both IL-4 production and membrane CD30 expression in established Th1 cell clones
Journal of Orthomolecular Medicine Vol. 10, No. 3 & 4, 1995
Adverse Effects of Zinc Deficiency: A Review from the Literature
Am J Obstet Gynecol. 1993 Dec;169(6):1456-61
Deficient glutathione peroxidase activity in preeclampsia is associated with increased placental production of thromboxane and lipid peroxides
Journal of Orthomolecular Medicine Vol. 5, No. 3, 1990
Mineral Imbalances in Pregnant Mothers and Their Newborn
Int J Fertil. 1987 May-Jun;32(3):192-3, 197-9
Progesterone therapy to decrease first-trimester spontaneous abortions in previous aborters
Biol Neonate. 1987;52 Suppl 1:78-86
Taurine and the premature
Archives of Environmental Contamination and Toxicology
Volume 3, Number 4 / December, 1975: 479-490
Prolonged ingestion of commercial DDT and PCB; effects on progesterone levels and reproduction in the mature female rat
Br Med J. 1954 November 6; 2(4896): 10711076
Similarity of Symptomatology of Premenstrual Syndrome and Toxaemia of Pregnancy and Their Response to Progesterone
BMJ DEC. 6, 1947
Vitamin-D Requirements in Pregnancy